Capping Illusions: Why limits on out-of-pocket drug spend don’t work.
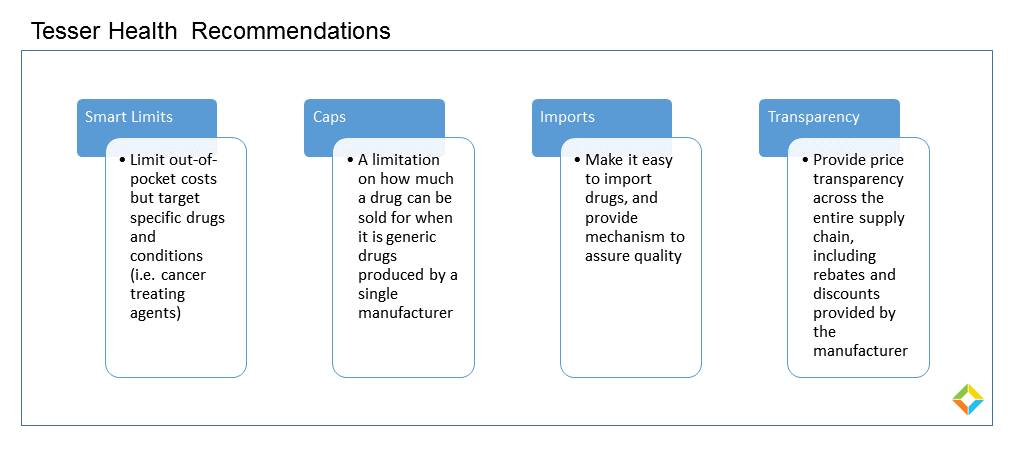
While a proposed cap on out-of-pocket drug spend seems to be the common response to the current drug pricing conundrum, in reality there are significant drawbacks.
On the surface, capping out of pocket drug costs seems like a great idea. Patients would no longer have to worry about paying exorbitant prices for their medications.
However, it is important to think about the repercussions of such a prescription drug plan that shields patients from the total cost of medications. This will give pharmaceutical manufacturers (both generic and name-brand) free rein to charge whatever they please for their drugs because the patient is no longer incentivized to choose more affordable medications or shop around for the best price.
One can make the argument that this can in turn drive generic and name brand manufacturers to increase the total cost of their drugs. Secondly, drug companies offer prescription assistance programs to help patients afford their medications. If a patient’s max cost is $250, the pharmaceutical companies will no longer need to fund these initiatives and will pass the financial burden of fully covering expensive medications to self-insured employers and payers.
Historically speaking the payers (pharmacy benefit manager) will either move expensive drugs off formulary (see Express Scripts & CVS after the Affordable Care Act) or pharmacies will refuse to sell certain drugs because the reimbursements are lower than the cost to acquire the medication.
Ultimately, capping out of pocket costs turns back the clock on all the progress made with consumer driven health plans. It will be interesting to see if this becomes reality and if so who will accept the financial burden.
Tags: cap, daraprim, drug prices, drug spend, expensive drugs, medications, out-of-pocket, out-of-pocket drug spend, price transparency